It all began with a chicken. Or at least, I think I can trace it back to a supermarket ready-meal I bought in 2007, in my third year studying radiotherapy and oncology at university. I contracted a food poisoning bug called Campylobacteriosis, and little did I know that this would set off a chain reaction of multiple organ systems failing.
 After 6 months, I began to have severe and frequent urinary tract infections (UTIs); as soon as I managed to clear one infection with a course of antibiotics, another would appear. One day I awoke with severe pain, and, despite trying every recommended step, I was unable to empty my bladder. The urology team put me on intermittent self-catheterisation (ISC) 12 times a day. Clamping and being in retention made this difficult, so I was switched to a urethral catheter.
After 6 months, I began to have severe and frequent urinary tract infections (UTIs); as soon as I managed to clear one infection with a course of antibiotics, another would appear. One day I awoke with severe pain, and, despite trying every recommended step, I was unable to empty my bladder. The urology team put me on intermittent self-catheterisation (ISC) 12 times a day. Clamping and being in retention made this difficult, so I was switched to a urethral catheter.
Bladder and bowel trouble
I wanted to carry on working, and somehow for a while I managed to run around a busy radiotherapy department with this bag attached to my leg. It didn’t last long, and I took the tough decision to hand in my resignation. Everything I had worked so hard for seemed to disappear in the blink of an eye.
‘Everything I had worked so hard for seemed to disappear in the blink of an eye’
Still, it was the right decision, as things only got worse. My body did not like the urethral catheter; it brought on horrendous spasmodic pain that felt like my bladder was giving birth to it. While these bladder problems were going on, my bowel also started to fail. It began to struggle with peristalsis, slowing movements and causing severe constipation. Soon I could only empty my bowels with laxatives, barium enemas and in the end a Peristeen irrigation system. Unable to eat normally, I became malnourished and very thin, as well as in horrific pain.
I was in A&E every 2–3 months with complications and catheter-induced infections. I felt unable to do anything, which began to take its physical, mental and spiritual toll.

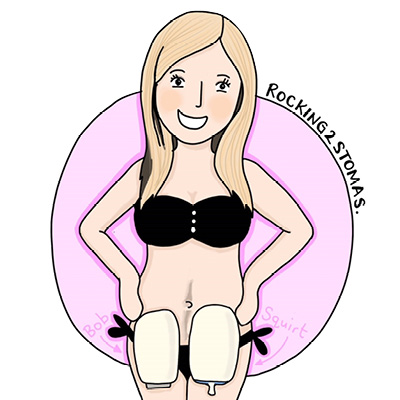
Rachel shows off her stomas for Rare Disease Day
New friends
Finally, in 2010, after really pushing my case forward, I received a supra-pubic catheter. This was easier to cope with and reduced the pain. However, I was still being misdiagnosed, and my case continued to stump the many top consultants I met. The not knowing that came with being put down as an anomaly felt like another battle in itself.
In June 2012, it was finally decided that I needed an emergency permanent ileostomy. Thus my life was saved, and Bob the Knob was born.

‘Being in hospital need not put life on hold’
Enter the neurologist
Later that year, a neurologist became involved. He was adamant I had a condition called autonomic neuropathy, and he chased the referral to the specialist unit at University College Hospital London. There I underwent a variety of weird and wonderful tests until I was diagnosed with pure autonomic failure (PAF), a type of autonomic neuropathy (dysautonomia).
‘I felt indescribable relief knowing this wasn’t all in my head’
I felt indescribable relief knowing this wasn’t all in my head and there was a reason why my organs were failing. However, this relief was outweighed by finding out that there was no cure, it was a progressive disease and I would be discharged becau se there was nothing more they could do.
Moving on
After discharge, I moved to glorious Bournemouth, where I have had wonderful care from all the various hospital departments. However, my bladder pain, bleeding and discomfort grew worse. Routine cystoscopy in July 2015 revealed that, not only was the bladder extremely small, it was so badly damaged that, according to biopsy results, the cells had started to mutate.
The only option was to have my bladder and lymph nodes removed and an ileal conduit (urostomy) formed. Within 2 weeks Bob was joined by Squirt the urostomy, named after the havoc he caused when the stoma nurse first changed him. The surgery went well, although I contracted another gastrointestinal bug, Clostridium difficile, from another patient, which lead to more complications and a 3-month isolated stay in hospital.
What's in a name?
When I tell people I’ve named my stomas, I tend to get the same blank looked, followed by laughter. Yet there is method to the madness. Naming a stoma gives this ‘thing’ an identity. An identity makes it something you can start to like, to form a personal relationship with and to accept as a friend keeping you alive. Where would I be today without my buddies Bob and Squirt?
Like any relationship, there is bound to be a bit of a love/hate dynamic going on, but if you can’t get rid of a stoma, you have to learn to live with it. If you have to get along to make the most of life, why not add a bit of humour to a ‘serious’ situation?
Double bagging
Still, the operation to swap the SPC for Squirt was the best decision I have ever made. Before, I was unableto walk, I endured horrific pain and I struggled mentally; this was not living, only existing. Waiting for surgery, I had been full of worry about what life would be like after. Yet, once I recovered, I realised quite how much freedom had been given back to me, and I maintain that my life has been a thousand times better since. There is naturally an adjustment period, but once you learn to look after your stoma you soon begin to accept it.
‘I maintain that my life has been a thousand times better since’
Don’t get me wrong; it hasn’t always been unicorns and rainbows. My ileostomy had a kind of prolapse called an ‘intussusception’, where part of the bowel has folded into itself .Eight surgeries over 18 months have failed to refashion it, which according to the consultant is apparently extremely rare and likely the result of Ehlers-Danlos syndrome, a rare genetic condition that weakens connective tissue. What is more, kidney disease has now taken surgery as an option off the table.
Ward life
Perhaps as a consequence of the prolapse, I have also had trouble with sepsis. I spent more than half of 2016 in hospital, which made my mere six admissions in 2017 feel like major progress. Not only have I come to accept that I might spend a significant part of my life in hospital, I believe that being in hospital need not put life on hold.
After 9 years of illness, I feel like I have achieved a degree, a masters and a PHD in being ill. Not only have my stomas saved my life, but they have given me a new sense of purpose. Thanks to the same illness that caused me to leave my medical studies, I have been able to find my focus speaking up and caring for the health of others. My aim is to raise awareness of issues urostomates and us double baggers face, especially among stoma companies, as well as to reach out to other ostomates in need.
The IBD & Ostomy Support Show
Watch on YouTube at The IBD & Ostomy Support Show, live every Thursday at 8pm, and follow on Facebook
Presenters


Reaching out
Being able to chat and share stories with other patients coming through the ward, especially those in for a stoma who have similar experiences, has helped me keep a positive outlook and make the most out of the situation. I have met many awesome ostomates, as well as an amazing man with a bag.
‘I have met many awesome ostomates’
I have been working with the Urostomy Association UK charity, and in January 2017 I started a blog, Rocking2Stomas, which you can follow on Facebook and Twitter. I also help co-present The IBD and Ostomy Support Show on YouTube, where I join Louise, Stephie, Natalie, Stephie and Steve to talk everything stoma in a friendly, informal setting. We go out live every Thursday at 8pm, and you can catch up on YouTube.
I can’t express how much helping others and advocating has moved me from self-pity to acceptance. The trials and tribulations of my chronic illness mean I have a story, and if this means I can help just one person to identify and feel they are not alone, then I have done my job.

I have met many awesome ostomates
 Rachel Jury blogs about life with two stomas as well as co-presenting The IBD and Ostomy Support Show on YouTube and raising urostomy awareness
Rachel Jury blogs about life with two stomas as well as co-presenting The IBD and Ostomy Support Show on YouTube and raising urostomy awareness
The contents of this page are property of MA Healthcare and should not be reused without permission

