I was in my late teens when I first started experiencing problems with constipation and abdominal pain. At that time, I was also dealing with anxiety and depression. It wasn’t until I turned 30 that I discovered my challenges were actually related to autism. Consequently, my GP attributed my gastrointestinal difficulties to stress. Although it wasn’t significantly affecting my life back then, it certainly posed an ongoing annoyance. As the years went by, the occasional bouts of constipation began to occur more frequently and intensified in pain. I distinctly remember a holiday visit to my aunt in Sheffield, during which I hadn’t been able to use the toilet for ten days. In response, she urgently rushed to a chemist for advice and returned with an enema, instructing me to stay close to the toilet due to its fast-acting nature. And indeed, it worked wonders—however, it wasn’t long before I found myself painfully constipated once again.
Subsequent trips to the GP led to a referral to a gastroenterologist at the hospital. This was during my early twenties, and I had never been under hospital care for health issues before. Consequently, I was unfamiliar with what to anticipate. Reflecting on this now, armed with the knowledge I possess, I realise I should have been more assertive about my needs. Following evaluations, the hospital diagnosed me with irritable bowel syndrome (IBS). They mentioned the option of undergoing endoscopies, but with no expectations of finding anything significant. Personally, I was vehemently opposed to any form of camera-based tests, so the matter was settled then and there. The GP then prescribed regular sachets of Movicol, an osmotic laxative designed to enhance water absorption in the bowel rather than exerting forceful stimulation (NHS, 2022). For a number of years, this approach worked effectively for me. This period coincided with my enrolment in college to pursue an Access to Higher Education Diploma in Social Studies, which I accomplished with distinction. Following this achievement, I embarked on my journey as a mature student at university that autumn.
Around this juncture, my suspicions about my condition being more complex than IBS grew significantly stronger. Although my GPs repeatedly assured me that IBS wouldn’t cause my bowel to abruptly cease functioning, I couldn’t shake off the idea that something was wrong. The familiar signs signalling the need to defecate were replaced by searing discomfort in my pelvis, abdomen, back and lower regions. It felt as though my insides were solidified, as if filled with concrete. Despite escalating dosages of osmotic laxatives, they ceased to be effective. Suppositories and enemas were introduced to complement my regimen, but the situation remained unchanged. The escalating physical and mental health issues forced me to discontinue my university studies after the initial year. This predicament led to growing despondency, as I found myself repeatedly unable to partake in outings due to the agony I was enduring. Two-week intervals without a bowel movement became the norm, punctuated confusingly by bouts of diarrhoea—a consequence of my backed-up bowel only allowing liquids to pass and ‘overflow.’
Frustration and desperation became overwhelming, propelling me to consent to a colonoscopy. I harboured a glimmer of hope that the procedure would unveil an easily treatable explanation for my distressing symptoms. However, even though I meticulously adhered to the preparation instructions, the bowel prep showed only partial results. The colonoscopy provided a limited view into my large bowel, ultimately yielding no findings of significant concern.
The pivotal moment in my journey unfolded in 2017. Having relocated from one local region to another, I found myself within the catchment area of a different hospital. My new GP referred me to a pelvic floor clinic at this hospital, where fate was on my side as my initial appointment was scheduled with a skilled colorectal surgeon who continues to oversee my treatment today. Right from the start, he grasped the enormity of the issue for me and the profound impact it was having on my daily life. He orchestrated a comprehensive series of tests that unveiled the presence of a severely slow transit not only within my colon but also in my stomach.
In response to this diagnosis, I embarked on pelvic floor physiotherapy. This approach aimed to instruct me in more effective ways to evacuate stool through biofeedback training. Regrettably, the benefits were limited, prompting me to delve into online research for alternative solutions. During this exploration, I stumbled upon accounts from fellow sufferers on Facebook who had achieved success with devices like the Peristeen anal irrigation system. This apparatus employed a catheter with a balloon to introduce water into the bowel, with the intention of flushing out stool.
Given the promising feedback, I was granted the opportunity to initiate this method. A compassionate bowel nurse from Coloplast came to my home to provide guidance on its usage. Initially, the Peristeen device yielded positive results, but in due course, akin to the previous interventions, its efficacy dwindled, and my pain intensified.
There were moments when I’d find myself lying on the bathroom floor, grappling with intense agony, and hoping for relief. My emotions were a mix of frustration and anger, directed not just outward, but also inward. I’d get frustrated with myself and the world around me. People with good intentions would offer suggestions about how they managed their IBS—had I considered laxatives, yoga, fybogel, or deep breathing? It was tough not to snap back, ‘Yes, I’ve tried them all, and nothing seems to make a lasting difference!’ At the age of 28, I often felt like I was at a dead end, as if life was slipping away. Yet, amidst it all, I still held on to a flicker of hope, even when I was worn out and couldn’t see a clear path forward.

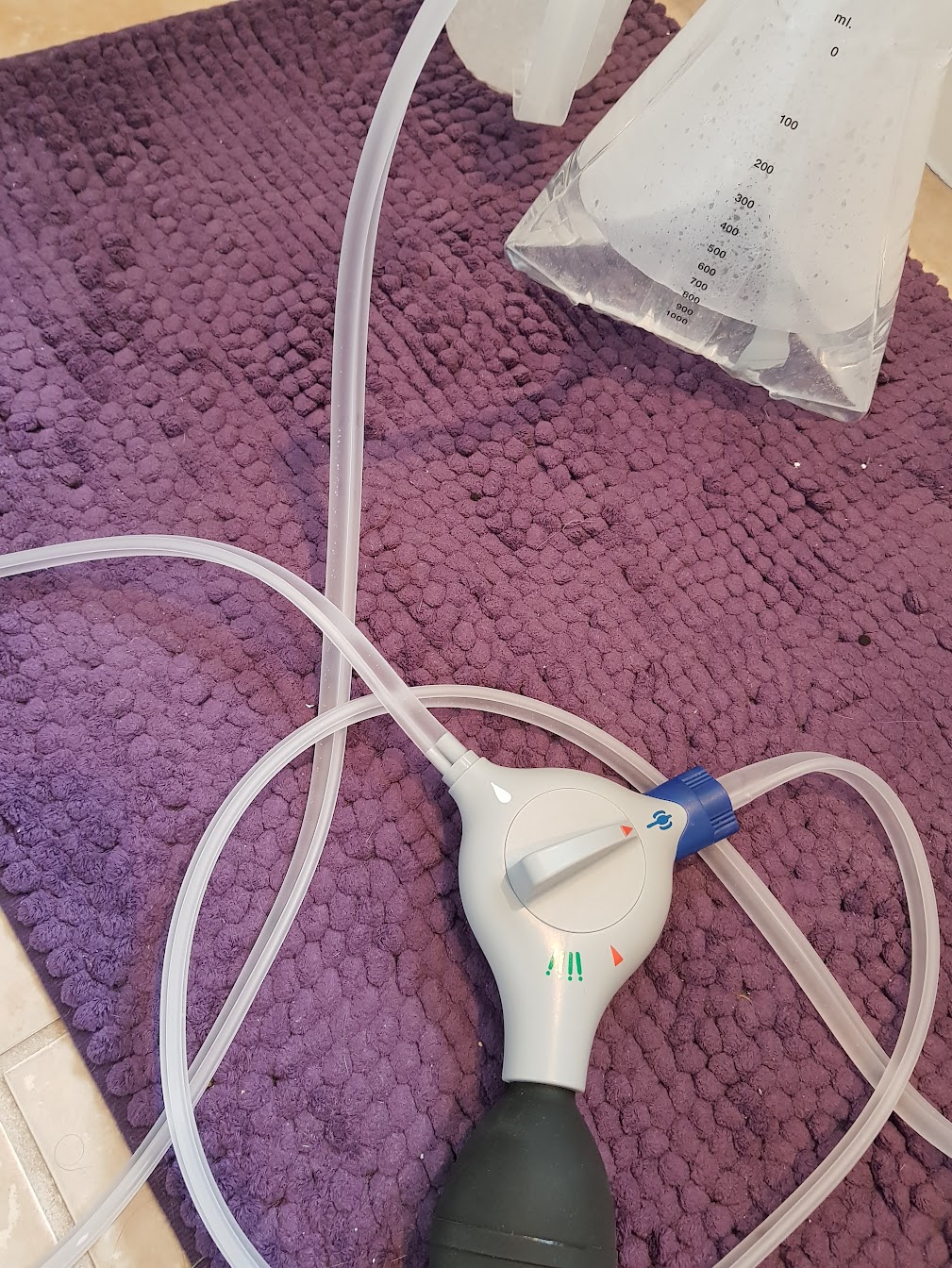 Sarah's peristeen irrigation kit (2017)
Sarah's peristeen irrigation kit (2017)
Once more, I found myself turning to the internet, finding stories of individuals with severe constipation and bowel dysmotility who had chosen to undergo an ileostomy procedure. While the notion seemed quite significant, I couldn’t ignore the fact that unless something drastic changed for me, my quality of life would remain stagnant. The consultant overseeing my case, who I initially met through the pelvic floor clinic, was also a seasoned colorectal surgeon. He undertook the task of seeking approval from the hospital to move forward with the surgery. The decision brought forth differing opinions within my family.
My mother was supportive from the get-go, possibly because of her experience caring for individuals with stomas. However, my father struggled initially to come to terms with my desire for a stoma. He held onto concerns that it might restrict me, associating stomas only with older people, and bought into misconceptions about their hygiene. It’s unfortunate that such myths still linger. I did my best to educate him, but ultimately, I recognised that the surgery was necessary for me, regardless of family opinions. Thankfully, my partner, Dave unwaveringly stood by my side, providing a solid foundation of support throughout the entire journey.
On the 23 May 2018, I underwent my ileostomy surgery! I wish I could say that everything went smoothly from that point forward, but life still had its share of ups and downs in store for me. However, I’ve never once regretted my decision to have the ileostomy. Shortly after the surgery, I encountered an issue known as ileus, where the small bowel doesn’t resume normal activity after the operation. This brought on considerable pain and vomiting, leading to the insertion of a tube through my nose into my stomach to release accumulated bile and alleviate pressure. Thankfully, after about a week, my small bowel gradually started functioning again, and my stoma came to life! I found myself captivated by its movements and would often spend time observing it. The sight didn’t disgust me, though I did experience frustration while learning to change and empty the bag. It wasn’t until I returned home and settled into my familiar environment that I truly got the hang of things and established a routine. The stoma nurses provided exceptional support, and I felt well-guided throughout the process. As my recovery progressed and my father witnessed the remarkable positive change in me, he too began to accept my choice to have the stoma.

 Sarah recovering from surgery (2018)
Sarah recovering from surgery (2018)
Following my stoma surgery, I made the decision to return to university with a newfound determination to finally complete my degree, after several earlier attempts had been cut short. A mere four months after my stoma surgery, I embarked on my journey in policing and criminal justice. At the outset, I had concerns that fellow students might hear unusual noises or spot a slight bulge on my abdomen. However, as it turned out, nobody noticed—truly affirming that having a stoma is virtually imperceptible unless disclosed. Even though I developed a parastomal hernia that I’m awaiting surgical correction for, I persevered and successfully finished my degree, ultimately graduating in 2021. Stepping onto the stage at the graduation ceremony stands out as one of the proudest moments in my life.
A couple of years following my stoma surgery, I underwent an assessment in London that finally provided me, at the age of 30, with answers about my health. It turned out that a genetic condition known as Ehlers-Danlos syndrome (EDS) was at the root of my health issues. EDS impacts the connective tissue found throughout the body, including organs. Instead of IBS, it was the EDS that was affecting my stomach and bowels, resulting in the intense pain and slow transit that eventually led to my ileostomy. This revelation was a tremendous relief, even though a part of me felt a sense of sadness at having been dismissed by doctors during the early years of my struggles with my bowel health.
 Sarah's graduation (2021)
Sarah's graduation (2021)
Having a stoma has actually improved my quality of life—it’s been the key that’s allowed me to truly live again! I enjoy trips to the cinema, theatre outings, and I’m able to go on holidays. To be prepared for any situation, I always carry ‘nappy sacks’ and wet wipes with me. These can be quite handy, especially when a toilet isn’t nearby, like on the motorway. I find myself needing to empty my bag quite frequently, but carrying an ‘I can’t wait’ card has proven helpful. Additionally, having a radar key provides access to disabled toilets, which has been invaluable.
Currently, I’m in the process of fundraising for a powered bike attachment for my wheelchair, which I urgently require to maintain my independence. Due to the strain it places on my joints and abdomen, I’m unable to self-propel, even once my hernia is repaired. Given my Ehlers-Danlos syndrome, I’ll remain at high risk for its recurrence. I’ve set up a GoFundMe page, and any small donation would be incredibly appreciated! You can find the page here: https://gofund.me/94335e6e

