For people living with a stoma, there are few things as important as looking after the skin around the stoma, known as the peristomal skin. Maintaining healthy peristomal skin can be the key to a comfortable life after surgery.
It’s important to be able to tell whether your peristomal skin is healthy, and you should check each time you change. Luckily, this is easy: your peristomal skin should look and feel the same as the rest of the skin on your abdomen (tummy). If it doesn’t—for example, if it is red, weepy, itchy or sore—you might have a peristomal skin complication. If you are unsure, you should contact your stoma nurse, as these issues are easier to resolve if detected early.
It might be complicated
Peristomal skin complications are unfortunately fairly common. Studies have found that up to 63% of ostomates will experience a skin problem within 3 months of surgery.1 These complications can be uncomfortable and/or painful, and they can make it harder to form a good seal with your pouch, while persistent skin problems can leave people feeling anxious, unhappy and isolated.
Fortunately, skin problems are not something anyone should have to put up with, and the great majority of these issues can be resolved. Far too many ostomates suffer in silence because they think that sore skin is part of living with a stoma. The truth is, once you’ve worked out what is causing a skin problem, there is almost always a way to fix it and avoid it coming back.
Peristomal skin complications are most commonly caused by prolonged contact with moisture and/or the stoma’s corrosive output. They can also be caused by excessive and/or aggressive removal of the baseplate of the pouch. Less commonly, problems can occur due to an allergic reaction, issues with body hair or a bacterial or fungal infection. All of these issues are resolvable, and this article will cover how they can be avoided, recognised and cleared up.
Speak with a nurse
Working out the cause of a skin problem and finding the best solution usually requires the assistance of a specialist stoma care nurse. If you notice any changes to do with your skin, you should get in touch with a stoma nurse right away. The sooner you do this the better, as skin problems are usually easier to resolve in the earlier stages, and you do not want to let the problem get worse.
The nurse will assess your stoma, your skin and your stoma care routine to determine the cause of the problem. It is important that you tell them about any changes in routine or any products you have used on your skin. Once the nurse has made an assessment, they can then recommend any changes that will correct the damage. This could be a simple change in stoma care technique. They may recommend that that you change your ostomy pouch (appliance or bag) to one with a different type of adhesive baseplate (skin barrier or flange) that may be more suited to your needs. If these don’t work, they may recommend that you try using additional supporting products, also known as stoma accessories.
No unwanted contact
The most common cause of peristomal skin complications is the skin under the pouch baseplate coming into long-term contact with moisture, particularly the output from the stoma. Specialists may refer to these conditions as irritant dermatitis or peristomal moisture-associated skin damage (PMASD).
The output of a stoma can have a major impact on the peristomal skin. Output from an ileostomy contains digestive enzymes that can start to break down the skin in a very short period of time. Urine from a ursotomy can also cause skin issues, especially if there is infection present.
Therefore, an effective ostomy pouching system will avoid this by making sure that the output goes straight into the bag without ever touching the skin. If the output does reach the skin, it means that here has been an unwanted leak. Avoiding or fixing PMASD usually means making adjustments to your pouching system until it forms a perfect seal and minimises the likelihood of leaks. Every stoma and every abdomen is different, and there are many different stoma care products designed to fit different body shapes.
Forming a perfect seal can be challenging. The pouch should sit as close as possible to the stoma. However, no two abdomens are the same, and, if there are scars, folds or creases, it can be difficult to achieve a complete secure seal around the stoma. Likewise, it can be made harder if your stoma doesn’t stick out enough (flush or recessed) or sticks out too far (prolapsed). However, there should be a pouching system for every body shape, and and even stomas on complicated abdomens should achieve a secure seal with the use of the right products.
The choice of product should take account of the shape of your abdomen, known as your body profile. For example, some body profiles might be better suited to a pouch with a convex baseplate, although you should only ever try this after discussion with your stoma nurse. Stoma paste can be sculpted into the folds of bumpy peristomal skin to give it a flat surface for the baseplate to stick to. Meanwhile, rings (sometimes called washers or seals) can help form a close seal around the stoma itself.
Remember that stoma output should not be making contact with your skin. There are many different manufacturers of stoma pouches and accessories and you may have to try several before you find the one that suits you and your stoma/skin. A good seal around your stoma and healthy skin reduce the need for clinical intervention and can increase quality of life.
Lift me gently
Another common cause of peristomal skin complications involves the pouch baseplate being removed too frequently and/or with too much force. Stoma care specialists refer to this as skin stripping or peristomal medical adhesive-related skin injury (PMARSI). If the adhesive barrier is stuck very firmly to the skin, removing it can cause trauma to the skin by pulling away at the outer layer. If this is done too frequently, it can cause more serious, lasting discomfort and damage.
To avoid this, the first step is to use the correct technique. A stoma nurse will teach you this when you are in the hospital; however, it may be something that needs to be revisited. They can also show your partner or carer the correct way if they are helping you. It helps to maintain some tension on the skin while peeling back the adhesive, starting at the top and working your way down. You should go slowly, because rapid removal increases the chance of stripping.
The next step is to minimise how frequently you have to remove the baseplate. If you are frequently replacing your pouch to fix a leak, it is essential to find a pouching routine that minimises the chance of these leaks happening in the first place. If you are using a closed pouching system and you are changing this two or three times per day, it may be worth considering a two-piece system, where the baseplate stays on the abdomen while the pouch is removed. This will reduce the potential for trauma on the skin. It is not advised to leave the baseplate on for longer than 3 days.
A two-piece pouch has a bag that can be detached from the baseplate; this allows the bag to be disposed of and replaced, while leaving the baseplate in place. A drainable pouch or separate baseplate will need to be removed every 2–3 days, especially as the hydrocolloid material, if left on too long, can break down and become harder to remove.
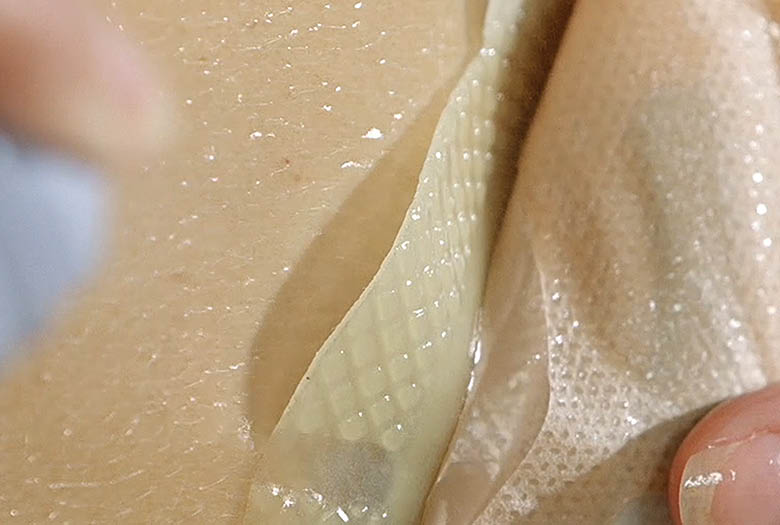
If these steps alone do not prevent skin stripping, you can try adding an adhesive remover to your pouching routine. These wipes and sprays weaken the adhesive’s bond with the skin, making removal easier, more comfortable and kinder to your skin. To use a remover spray, peel back a small part of the edge of the adhesive, spray a little remover onto the skin and allow it to gradually run behind the baseplate until the pouch comes off easily—do not spray it over the top of the pouch. Adhesive removers are often a valuable tool, as they can help reduce trauma to the skin during pouch removal.
The cause of the problem may not always be obvious, and your stoma nurse may swab your skin and send it for testing to see if the there is an infection present.
Adhesive remover
Water, water everywhere
One of the key tools for maintaining healthy peristomal skin is water. You should clean around your stoma using plain water, with no soaps or other skincare products. This is because these products can interfere with the pH balance (acidity) of your skin, which can leave it more vulnerable to infection. After cleaning the peristomal area, you should gently dry the skin before applying the adhesive baseplate.
It is also important to drink plenty of water to keep y our skin hydrated, because the skin cells need water as nourishment to renew themselves. Normally, this should be around 1.5–2 litres of fluid each day, but it should be more if you are doing a lot of physical exercise, which will cause you to lose more water as sweat. If you have an ilesotomy, your fluid intake should be greater to account for the fluid losses in your output. It should be noted that too much sweat trapped under the baseplate of a pouch can contribute to skin breakdown, but an effective pouching system should be able to keep moisture levels under control.
A close shave
Peristomal skin irritation can occasionally be a result of inflammation and/or infection of the hair follicles, known as folliculitis. Folliculitis can be caused by removing the adhesive baseplate in a way that pulls the hairs out of the skin, as well as bacteria trapped in the follicles.
If you have a lot of hair growing around your stoma, you may wish to reduce the chance of folliculitis by shaving the area carefully. Shaving in the direction of the hair may help prevent inflammation. If you have red bumps around your stoma, a stoma nurse can swab the area to test for infection.
Conclusion
The most important message to take away from this article is that you do not have to live with sore peristomal skin. If you suspect a problem, seek advice at the earliest opportunity from your stoma nurse.
Healthy skin is key to living well with a stoma, and it should be an achievable goal with the right support, products and techniques.
Sources
1Salvadalena GD. The incidence of stoma and peristomal complications during the first 3 months after ostomy creation. J Wound Ostomy Continence Nurs. 2013; 40(4):400–406
Sue Pridham is Ostomy Nurse Manager for Amcare Nuring Group (Convatec/Amcare group)

